Tom’s takeaway: Depression and anxiety are common in people with pain, and exercise is uniquely helpful to help manage the frustration, fatigue, and changed mood of persistent pain. Don’t wait till you feel better to exercise: exercise will make you feel better. If you exercise and do not feel the reported benefits – try changing the intensity, duration, location, music used, social level, or type of exercise.
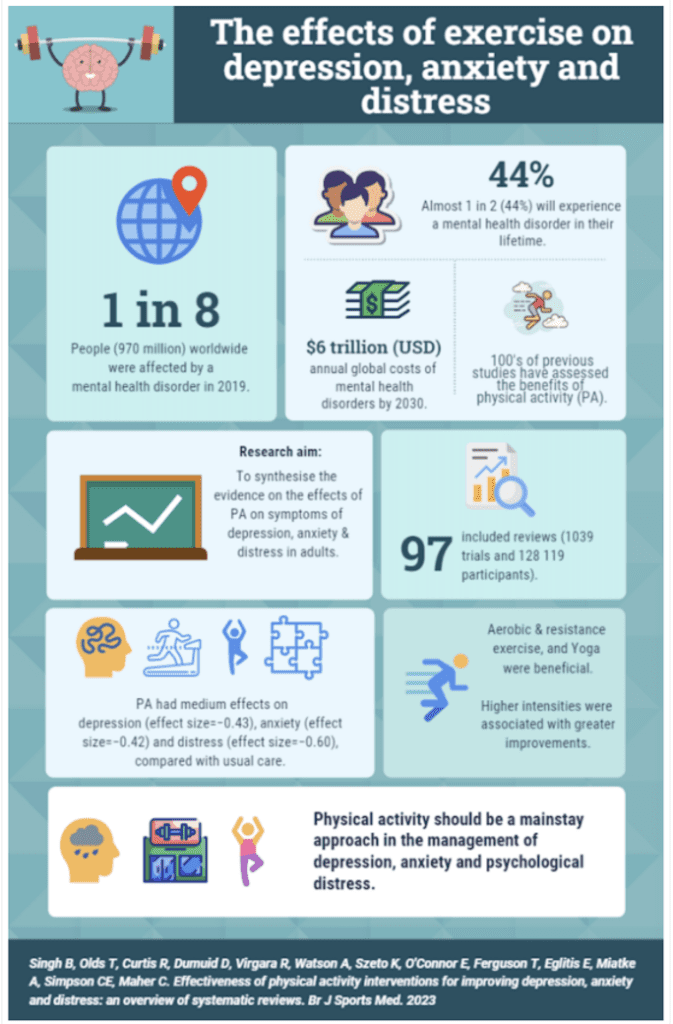
Almost half of us globally could be diagnosed with a mental health issue, which has been worsened for some people by the COVID-19 pandemic. This is important as, apart from affecting your quality of life, depression (for example) may increase the risk for cardiovascular disease, weight gain, and diabetes. For the last 10 years, it has been known that exercise helps reduce persistent pain while reducing the common side effects of depression and anxiety. This recent meta-analysis (a study of over 19 studies) showed positive effects of exercise training on reducing depression and anxiety, with greater effects seen for people with back pain and anxiety. The positive effect of exercise was also seen for people with both depression and anxiety.
Another recent meta-analysis showed even more positive effects of exercise across 1039 trials and 128 119 individuals. These included people without pain, pregnant and postpartum women, and those with neurological conditions (Multiple Sclerosis, dementia), kidney disease, and HIV. Higher levels of depression had greater benefits from regular exercise. Better effects were seen with higher-intensity exercise across the studies assessed. Of interest, more time spent exercising did not equal better results, unlike other health benefits such as aerobic fitness or muscle growth, where benefits gained are mostly dose-dependent. Shorter, harder exercise might be easier to comply with in the long term or cross a threshold that causes neurological and hormonal effects. For aerobic exercise, that might mean exercise where you can’t hold a conversion or sing; for strength training, when a set finishes with momentary failure completing a repetition. Some of these studies showed exercise had better mental health outcomes than medication or psychotherapy. Strength training on its own has significant effects on improving depression or anxiety, including in young adults.
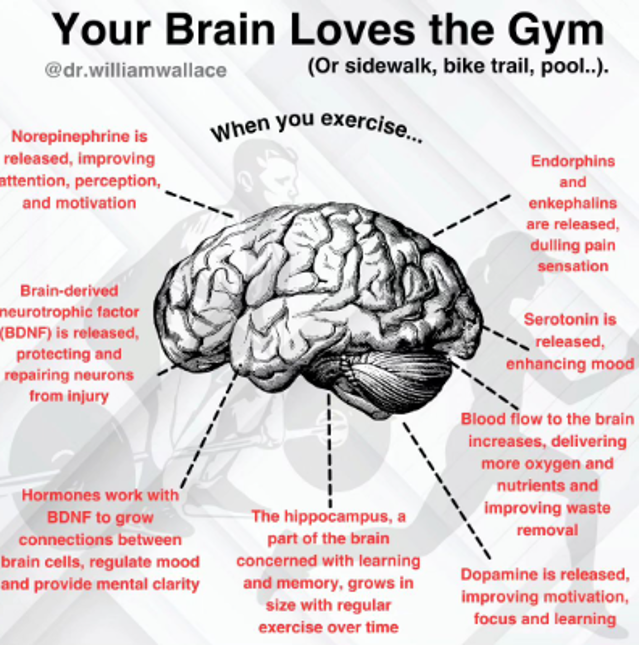
Exercise seems to improve depression through similar neuromolecular pathways to those targeted by antidepressant medication, i.e., increasing a combination of brain‐derived neurotransmitters or chemicals you might have heard about. These include serotonin, dopamine, opioid-based endorphins, and endocannabinoids (brain-made chemicals with properties similar to medical cannabis). Also, exercise reduces systemic inflammation and improves the functions of the areas of the brain that regulate emotions (such as self-esteem), mood, and perception of fatigue. Also another older theory is that increasing temperature in brain centers improves relaxation and perception of muscle tension. This might be part of how an exercise session “warm-up” that includes some form of low-intensity movement improves the perception of muscle tightness rather than changing tissue structure in the short term. Exercise also helps many aspects of other health outcomes, such as metabolism, sleep, and cardiovascular health. Overall, this study found that all modes of exercise, including strength training, Qigong, Pilates, yoga, and Tai Chi, have positive effects on people with musculoskeletal pain, depression, and anxiety. Therefore, it is recommended that clinicians who help people with mental health issues encourage these interventions as early after diagnosis as possible.
Evidence-based exercise specialists might be criticised for criticising other interventions labeled as “alternatives.” Ironically, in the mental health field, exercise therapy itself used to be considered an alternative medicine. However, the evidence is sufficient to offer exercise as an anti-depressive therapy. Still, it is often overlooked due to “patient resistance” and doctors’ difficulties prescribing and monitoring physical activity in clinical settings. “Patient resistance” might come from people waiting to exercise when “feeling better” or feeling like more time spent exercising is better. Again, the meta-analysis described here shows that the duration of exercise might not be important, so if the reader has a history of depression or is supporting someone with depression, we encourage you to reframe your thoughts from “need to feel better to exercise” to “need to exercise to feel better.”
Exercise is medicine for depression or anxious thoughts, so take a daily dose. All exercise modes are effective, and higher intensity is associated with more significant benefits. Find any exercise mode you want to start with, especially something social (which might have additive mood-boosting effects for some) and structured weekly. Reflect on your exercise habits and other lifestyle management approaches, such as pre-sleep habits and maintaining a healthy diet, and seek help from the clinicians at ACE. While short-duration high-intensity exercise shouldn’t be viewed as a replacement for other established treatments, exercise can be used as an additional form of treatment, reducing the risk of future relapses and counteracting weight gain commonly reported as a medication-related side effect. Resolve to progress gradually to meet larger recommended weekly doses of physical activity (see here for Australian PA guidelines) and also address other health conditions that accompany most anxiety and depressive disorders.
Written by Tom Murphey, DPT.
“Unfortunately for our community, scientific scaremongering is common, easy to believe, and hard to heal. Research is often messy, and strong stances or beliefs can be erroneous and dishonest. I aim to produce honest reviews of high-quality research to provide informed insight so you can make up your own mind on the science you value.”
References.
https://psychwestwa.com.au/psychology-services/acceptance-and-commitment-therapy
https://www.tamethebeast.org/#tame-the-beast
https://www.youtube.com/watch?v=L4cKCezBeLw Demystifying Depression in Older Adults

Comments:
share